Baldness, or alopecia, affects huge numbers of people all over the world. It can vary from male pattern baldness (in which the hair thins out gradually) to alopecia universalis (that is a total lack of all body hair). Alopecia is an equal opportunity condition, affecting both men and women across races, socio-economic statuses and age. For instance, UK actor Joseph Gatt (recently seen as an Thenn wildling on HBO’s Game of Thrones) developed alopecia universalis at the age of 14.? Various kinds of alopecia have different causes.
Alopecia areata (a common autoimmune disease) is characterized by patches of baldness, which BBC News health reporter Smitha Mundasad says affects roughly two in every 1,000 UK citizens. This is the type of alopecia that researchers at Columbia University School of medicine (CUMC) recently been studying. They’ve identified the immune cells responsible for destroying follicles of hair and also have developed and tested a brand new, FDA-approved drug that eliminated the immune cells and restored hair regrowth in a tiny number of patients. Their answers are described in a recent issue of Nature Medicine.
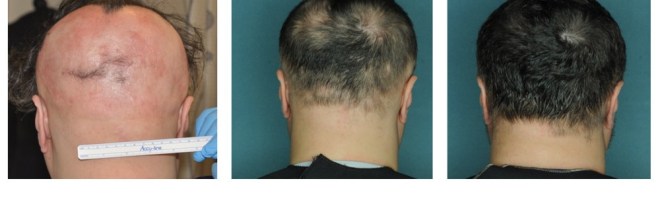
The researchers, including Raphael Clynes, MD, PhD, and CUMC professor in the Departments of Dermatology and of Genetics and Development Angela M. Christiano, PhD, report early results from an ongoing medical trial from the drug. These results include complete hair regrowth in several patients with moderate-to-severe alopecia areata. The report includes data from three participants, each of whom experienced total hair regrowth within five months of beginning treatment.
“We’ve only begun testing the drug in patients, but if the drug remains successful and safe, it’ll have an impressive positive effect on the lives of people with this particular disease,” said Clynes.
The hair loss from alopecia areata can be disfiguring, as it is often lost in patches on the scalp, face and the body. Up to now, there aren’t any known treatments that can completely restore hair. People with this condition often suffer from significant psychological stress and emotional trauma.
The mechanism for hair thinning – your hair follicle being surrounded and attacked through the immune system, causing the follicle to enter an inactive state – has been known for many years. Which particular immune cell was responsible, however, remained a mysterious. Four years ago, Dr. Christiano’s genetic study of more than 1,000 patients with alopecia areata uncovered the first major clue – your hair follicles send a “danger” signal, not previously associated with alopecia areata, which pulls the immune cells to the follicle and provokes the attack.
The current study initially started by studying mice with alopecia areata, tracking back in the danger sign to identify the specific set of T cells that initiate the attack. Follow-up examinations of both mice and human cells revealed how the T cells attack, and suggested possible pathways to be targeted with a new type of drugs called JAK inhibitors.
The team tested two FDA-approved JAK inhibitors separately: ruxolitinib and tofacitinib. Both could block the immune pathways and prevent the attack on hair follicles. Mice with extensive hair thinning in the disease had full hair restoration within 12 weeks with both drugs. Your hair persisted for several months after treatment was stopped with both drugs, as well.
The researchers collaborated with Julian Mackay-Wiggan, MD, MS, director from the Clinical Research Unit within the Department of Dermatology at CUMC along with a practicing dermatologist at NewYork-Presbyterian/Columbia who treats patients with multiple kinds of hair loss to initiate a little open-label medical trial of ruxolitinib, because it already had FDA approval to treat a blood disorder. The participants, seven women and two men, had moderate-to-severe alopecia areata with more than a 30 percent hair thinning. Within four to five months of beginning treatment, three of the participants saw complete hair restoration, combined with the disappearance from the attacking T cells from the scalp.
“We still need do more testing to establish that ruxolitinib should be used in alopecia areata, but this is exciting news for patients and their physicians,” Dr. Clynes said. “This ailment has been completely understudied-until now, only two small numerous studies evaluating targeted therapies in alopecia areata have been performed, mainly due to the possible lack of mechanistic understanding of it.”
“The timeline of moving from genetic findings to good results in a clinical trial in only 4 years is astoundingly fast and speaks to this team’s ability to perform translational science of the highest caliber,” said David Bickers, MD, the Carl Truman Nelson Professor of Dermatology and chair from the Department of Dermatology at CUMC and dermatologist-in-chief at NewYork-Presbyterian/Columbia. “There are few tools in the arsenal for the treatment of alopecia areata that have any demonstrated efficacy. This is a major advance in increasing the standard of care for patients struggling with this devastating disease.”
Dr. Christiano, who is affected with alopecia areata herself, says that it is all too often dismissed as simply an appearance altering condition. “Nothing might be further from the truth,” she said. “Patients with alopecia areata are suffering profoundly, which findings mark a significant step forward on their behalf. They is fully committed to advancing new therapies for patients with a vast unmet need.”
The New York Times cautions, however, the treatment will not work for everyone, and never enough is famous yet of side effects or safety concerns. Dr. George Cotsarelis, a dermatologist in the University of Pennsylvania, agrees that people should approach this “cure” with caution. The study participants received the drug like a two times a day pill instead of a topical cream, meaning that they were “treated systemically with a very toxic drug” known to cause liver and blood problems, infections and other negative outcomes. Dr. Cotsarelis said that if the drug could be applied topically, it might “be an amazing breakthrough.”
The team intends to continue larger numerous studies, that will range from the other JAK inhibitor, tofacitinib – originally approved for rheumatoid arthritis symptoms.